BREAST AUGMENTATION MASTOPEXY
An Augmentation Mastopexy is a procedure that combines a mastopexy with breast augmentation using implants. This combined approach may be considered for individuals who wish to address both a change in breast position and a loss of volume.
Understanding the Procedure
With age, weight fluctuations, pregnancy, or breastfeeding, some individuals may notice changes in the shape and position of their breasts. A common concern is breast ptosis, a condition where the breast tissue and nipple sit lower on the chest wall than desired.
The key consideration when planning this procedure is the position of the nipple in relation to the breast tissue. In some cases, the breast tissue may sit in the lower part of the breast, and the nipple may point downward or sit below the breast fold. This may create an elongated appearance when viewed from the side.
An augmentation mastopexy may aim to:
- Elevate the nipple to a more central position on the breast mound
- Adjust the skin envelope and internal breast tissue
- Restore volume through the use of implants
Tailored to Individual Needs
The surgical approach will depend on several factors, including:
- The amount of existing breast tissue
- The degree of ptosis
- Skin elasticity and chest wall anatomy
- Whether an individual desires an increase in breast size, correction of asymmetry, or both
When Breast Augmentation Alone May Be Suitable
In patients without significant ptosis, breast augmentation alone may be considered. This procedure involves the placement of an implant (round or anatomical/teardrop-shaped) to increase breast volume. Implant selection and surgical technique are based on the individual's chest anatomy, tissue characteristics, and surgical goals, which are discussed during a clinical consultation.
Mild Ptosis: Assessment and Management
A simple method sometimes used during examination is the arm-raise test. If, when the arms are raised, the nipple moves to a more favourable position and the lower breast tissue appears more elevated, then augmentation alone may still be a suitable option.
In such cases, additional surgical adjustments may be needed to support the breast tissue and position the implant correctly. An anatomical (teardrop-shaped) implant may be recommended to provide a more gradual slope and better fit with the existing tissue distribution. However, the choice of implant and surgical plan should be tailored to the patient's individual anatomy and preferences after a thorough assessment.
Moderate to Significant Ptosis: Augmentation Mastopexy
If the nipple remains low on the chest wall when the arms are raised, and the breast tissue continues to sit below the inframammary fold, a combined procedure called an augmentation mastopexy may be indicated. This involves:
- Placement of a breast implant (usually under the muscle)
- Repositioning of the breast tissue and skin envelope to elevate the nipple and reshape the breast
This approach allows for improved control of nipple position and soft tissue support but involves additional incisions and scarring compared to augmentation alone.
Staged Approach for Larger Implants
In some cases—particularly where a significant increase in breast volume is planned—a staged procedure may be advised. This means:
- A mastopexy is performed first, allowing tissues and scars to settle.
- Implant placement is carried out at a second stage, generally at least 3 months later.
This approach may reduce the risk of complications such as poor wound healing, implant malposition, or excessive scar tension.
Alternatives to Implants
For individuals who do not wish to increase breast volume significantly, a mastopexy alone may be appropriate. In some cases, fat grafting can be used to add moderate volume using the patient’s own tissue. This may be done alone or in combination with a mastopexy, depending on the goals discussed during the consultation.
Clinical Overview: Mastopexy with Augmentation Techniques
Breast augmentation mastopexy is a procedure that combines a mastopexy with the insertion of breast implants to address both loss of volume and changes in breast position. There are several surgical approaches available depending on the degree of ptosis, tissue characteristics, and individual patient factors.
1. Traditional Augmentation Mastopexy (Single or Staged Approach)
This method involves elevating the breast tissue and inserting implants during the same surgery, or in two separate stages depending on clinical need.
- Single-stage procedures may be suitable for selected patients with moderate tissue laxity and stable skin quality.
- Two-stage procedures (mastopexy followed by augmentation) may be advised when more significant adjustments are needed, particularly when larger implants are desired or skin quality is poor.
This technique allows for adjustment of nipple position, reduction of excess skin, and increase of breast volume through implant placement.
2. Peri-Areolar Mastopexy with Augmentation
This approach involves an incision around the areola and is typically suitable for patients with mild breast ptosis.
- The nipple-areolar complex may be repositioned slightly, and breast implants are inserted during the same procedure.
- Due to the limited nature of a mastopexy, it is generally reserved for patients not requiring extensive tissue repositioning.
- Scarring is typically limited to the areolar border, though scar visibility and healing vary between individuals.
3. Vertical Mastopexy with Augmentation
This procedure includes:
- A circular incision around the areola
- A vertical incision extending from the areola to the inframammary fold
This method is used in cases of moderate breast ptosis and allows for removal of excess skin and reshaping of the breast tissue. Implant placement is performed in the same operation, with adjustments made to ensure appropriate implant positioning and support.
4. Inverted-T (Anchor) Mastopexy with Augmentation
For patients with significant breast ptosis or excess skin, the anchor-shaped incision pattern may be used. This includes:
- An incision around the areola
- A vertical incision down to the breast fold
- A horizontal incision along the inframammary crease
This technique allows for the most extensive skin removal and tissue repositioning. Implant insertion is performed during the same operation and tailored to the patient’s anatomical needs and surgical goals.
Important Considerations
- The selection of technique depends on factors such as breast volume, skin elasticity, degree of ptosis, and patient preferences.
- Implant type, size, and placement (subglandular or submuscular) will be discussed during consultation based on physical assessment.
- All surgeries carry risks, including infection, bleeding, scarring, changes in nipple sensation, and implant-related complications. These should be discussed thoroughly with your specialist plastic surgeon.
- Recovery time, scar pattern, and postoperative care will vary depending on the chosen surgical approach.
Best Practices in Surgery
- Use of the 14-point plan of infection prevention
- Use of the Keller funnel. This is used to insert the implant with minimal contamination and shortest possible scar. It has become the new standard in breast implant surgery, aiming to minimise risk of capsular contracture. You will be able to see and feel the funnel during your consultation.
- Prevention of breast implant animation (through careful muscle dissection)
- Prevention of bleeding through meticulous haemostasis
- Special blocks to prevent post operative pain
- Use of the internal bra sutures. These are used to anchor the tissues down to near the rib cage. These reinforce the inframammary fold which help prevent implant migration downwards with time.
- Use of fat grafting as needed.
Potential Risks – Breast Augmentation Mastopexy
As with any surgical procedure, breast augmentation mastopexy carries risks. These include general surgical risks as well as those specific to combined mastopexy and augmentation surgery:
- Infection at the surgical site, which may require antibiotics or further treatment
- Bleeding or haematoma (collection of blood under the skin)
- Changes in breast shape, size, or symmetry following surgery
- Scarring, which can vary depending on incision technique and individual healing
- Altered sensation in the breast or nipple area, which may be temporary or permanent
- Capsular contracture (scar tissue formation around the implant), which may affect breast appearance or require further surgery
- Implant-related complications, such as rupture, leakage, or displacement
- Nipple or skin necrosis (rare), due to compromised blood supply
- Seroma formation (fluid accumulation), which may require drainage
- Persistent pain or discomfort beyond expected recovery time
- Anaesthetic-related risks, including allergic reaction or respiratory complications
Recovery and Aftercare – Breast Augmentation Mastopexy
- Swelling, bruising, and mild to moderate discomfort are common and usually improve over several weeks
- Pain relief may be prescribed or managed with over-the-counter medications as directed by your surgeon
- Dressings and wound care instructions should be followed carefully to promote healing and reduce infection risk
- Supportive bras or compression garments are typically recommended for several weeks to support the breasts and minimise swelling
- Strenuous activity, heavy lifting, and upper body exercise should generally be avoided for 4–6 weeks, or as advised
- Driving can usually be resumed once you are off prescription pain medication and feel physically capable of doing so safely
- Incision scars will fade over time but may remain visible; your surgeon may suggest scar management options
- Follow-up appointments are important to monitor healing, assess outcomes, and address any concerns
- Smoking and alcohol should be avoided during recovery, as they may impair wound healing
- Final results may take several months to become apparent as swelling subsides and tissues settle
If you have any questions or wish to discuss breast augmentation mastopexy options, please contact our clinic to schedule a consultation with Dr Reema Hadi.
For more information on Breast Augmentation Mastopexy, you can visit the Australian Society of Plastic Surgery
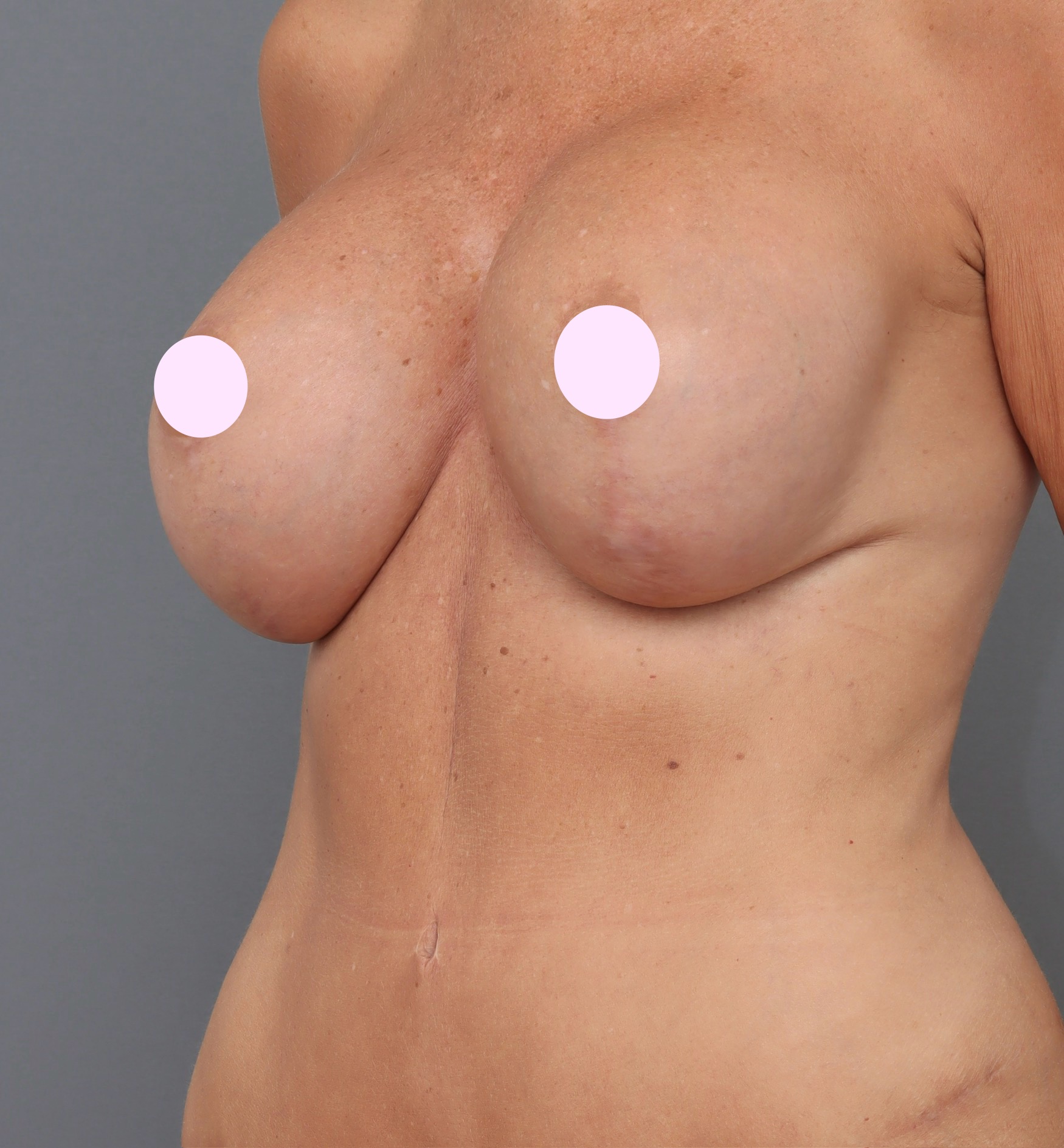
Before and After Photos
Real patient results from our expert procedures